Attend events on using your public health degree in the workforce, negotiate a salary offer, use AI for the job search, and more.
UW PUBLIC HEALTH MAGAZINE
Together we are ready
Community trust and health infrastructure are necessary to prepare for future public health crises



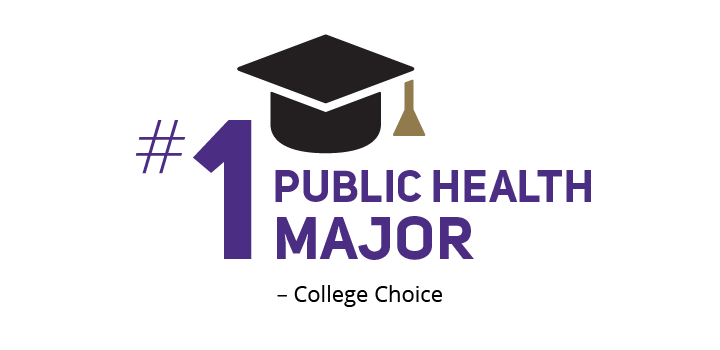
#7 in graduate education
UW SPH maintains its top-ten ranking in graduate public health education, according to US News & World Report