A breakthrough to speed COVID-19 vaccine research
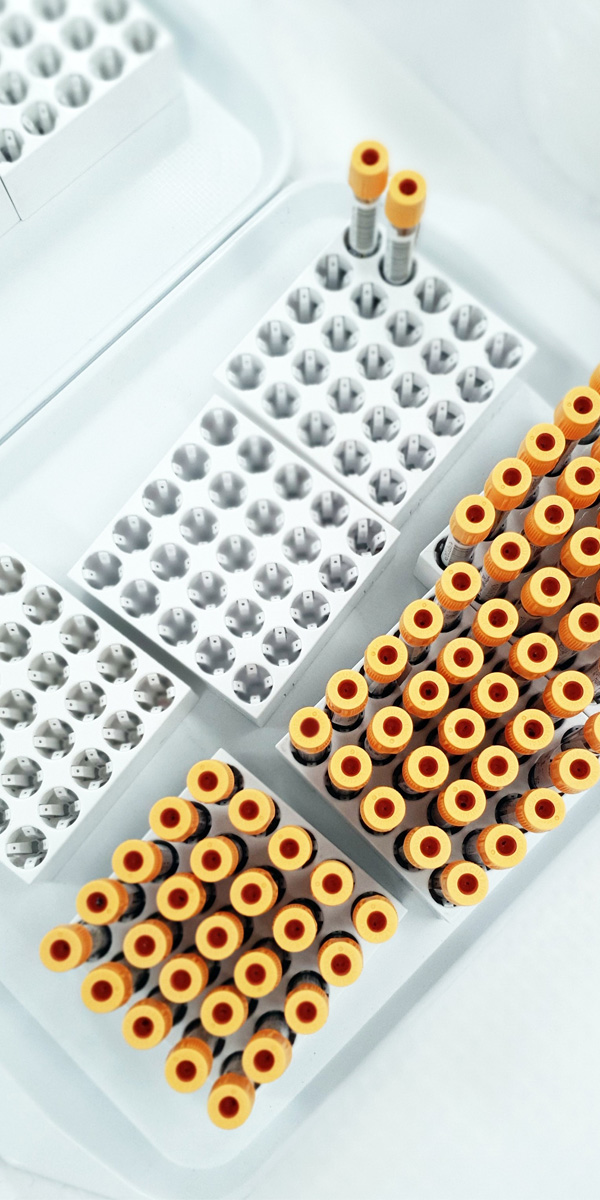
UW researchers made national headlines when they discovered that measuring certain markers in blood could determine protection against COVID-19 after vaccination.
These markers may enable researchers to speed prediction of how well a new COVID-19 vaccine would work, before or without conducting large-scale, time-consuming clinical trials.
“Our data support that these markers can be used to predict vaccine efficacy,” said Peter Gilbert, a professor of biostatistics in the UW School of Public Health. Gilbert, who led the breakthrough, anticipates that a clinical trial employing the markers to test future uses of vaccines might require only hundreds instead of thousands of participants.
The findings arose from analysis of blood-draw data collected during Moderna’s large clinical trial to test its COVID-19 mRNA vaccine. Gilbert and his colleagues homed in on antibodies — small proteins involved in the immune system’s response to the vaccine — and found that concentrations of certain types of antibodies tended to be lower in vaccinated people who later got COVID-19 than in those who didn’t. Their data analyses supported that higher antibody levels can serve as markers of greater protection against COVID-19.
“It’s definitely a seminal study in the cumulative body of evidence that these markers can be used to make certain vaccine-related decisions,” Gilbert said.
The work has already influenced research. Based in part on the findings, the Food and Drug Administration approved a streamlined study design known as “immunobridging” for Moderna’s tests of its vaccine in children. The findings are also shaping decisions on COVID-19 mRNA vaccine boosters.
“Measurement of these markers is one of the pillars of evidence that is being used by advisory committees to guide their recommendations of when to change the virus strains inserted into the vaccines and which strains to use,” Gilbert said.
He and his colleagues, including Affiliate Associate Professor of Biostatistics Youyi Fongare, are now testing whether the same markers apply to COVID-19 vaccines that, unlike the Moderna and Pfizer vaccines, are not mRNA-based. They recently reported findings that the same markers do in fact hold for Johnson & Johnson’s nonmRNA vaccine.
“This brings us one step closer to one of our ultimate long-term goals, which is a marker that can predict protection across vaccine platforms,” Gilbert said.
Joining forces to build coastal disaster resilience

UW researchers have partnered with other Pacific Northwest scientists and coastal communities on a novel research initiative that aims to build resilience to earthquakes, tsunamis and climate-change hazards — including coastal erosion and flooding.
Based at Oregon State University and co-led by the UW, the new Cascadia Coastlines and Peoples Hazards Research Hub integrates the perspectives and knowledge of communities near the Cascadia Subduction Zone, an offshore fault that could one day cause a megaquake.
“Our hope is to have a better understanding of the hazards coastal communities face; the strengths and vulnerabilities of their built, social and natural environments; and how communities can best prepare,” said Nicole Errett, assistant professor of environmental and occupational health sciences and part of the hub’s leadership team.
Errett and her colleagues will collaborate with tribes, government officials, community leaders, residents and other stakeholders to develop culturally relevant risk-mitigation strategies.
identifying disparities in vulnerability to hazards and engaging underrepresented populations. “It’s about joining forces with communities and being guided by what they need,” Errett said.
Debt harms health and well-being

Unsecured debt — such as credit card debt, student loans, or medical debt — increasingly harms people’s health and well-being in the U.S., according to a policy statement co-authored by Anjum Hajat, associate professor of epidemiology at UW School of Public Health in collaboration with Kirsten Wysen from Public Health – Seattle & King County and Elizabeth Sweet from University of Massachusetts Boston.
The statement, published through the American Public Health Association (APHA), outlines this complex and growing problem, highlighting adverse health impacts including anxiety, depression, and high blood pressure, while also exploring issues such as unfair lending practices that disproportionately affect women, people of color and other populations.
Nonetheless, mounting evidence supports specific strategies for addressing debt and its public health effects. Drawing from that evidence, the authors recommend 13 action steps. For instance, they call on the federal government to reduce current levels of debt in coordination with new policies to protect consumers from taking on excess debt. They also urge health departments to intervene in financial policies and products that harm health, and they suggest that health care providers refrain from ownership or investments in debt collection agencies. Such efforts could ultimately improve mental and physical health outcomes for Americans.
Setting the stage for global pediatric Shigella vaccines

Every year, a type of bacteria known as Shigella causes an estimated 60,000 deaths of children under five. Shigella is a leading cause of childhood diarrhea, and infection may trigger life-threatening complications and long-term health and nutritional problems.
Now, Patricia Pavlinac, assistant professor of global health at the UW School of Public Health, is leading an international collaboration to better understand the incidence and impact of Shigella diarrhea. Funded by the Bill & Melinda Gates Foundation, the Enterics for Global Health (EFGH) Shigella surveillance study is setting the stage for large clinical trials of promising Shigella vaccines.
“Understanding the underlying disease burden and preparing laboratory and clinical teams to identify and characterize children with Shigella diarrhea are critical steps to ensure the rigor of future vaccine trials,” Pavlinac said. “Moreover, when a vaccine is proven to be safe and efficacious, policymakers will need to weigh the cost against the benefit, and EFGH will be generating data to inform that value proposition.”
Pavlinac and her colleagues in Bangladesh, the Gambia, Kenya, Malawi, Mali, Pakistan and Peru have established a multi-country surveillance network. At each site, researchers will determine the incidence of Shigella diarrhea in children under three and collect additional key metrics, including children’s disease severity, outcomes and costs to families and health care systems.
“EFGH investigators are world experts in pediatric diarrhea,” Pavlinac said. “They contribute not only scientific expertise around the important research questions that need to be answered in this field, but also bring tremendous experience of managing children with diarrhea and implementing rigorous research studies, including vaccine trials.”
The findings should enable EFGH sites to hit the ground running when vaccine trials launch — which could begin as soon as 2024. Ultimately, Pavlinac and her EFGH colleagues hope the study will accelerate rollout of Shigella vaccines for children in low- and middle-income countries.
“Having such a wide network of collaborators ensures that we are collating diverse perspectives on how best to address Shigella and how to collect data that is maximally likely to make an impact of reducing the burden of childhood diarrhea,” Pavlinac said.
Supporting rural public health staff with data

Health disparities affect the well-being of people in rural communities, but many rural public health professionals lack the resources and access to data for addressing these challenges.
To help close that gap, the Northwest Center for Public Health Practice, housed in the UW School of Public Health’s Department of Health Systems and Population Health, partnered with public health agencies to build an online resource called Solutions in Health Analytics for Rural Equity across the Northwest (SHARE-NW).
SHARE-NW features dashboards that put key data that they requested at the fingertips of rural public health professionals, supporting them in their efforts to identify and communicate health inequities with community members and decision or policymakers. Aimed at rural professionals in Washington, Alaska, Idaho and Oregon, the website provides local data across the region and in several public health topics, including obesity, mental health and violence prevention. It also includes free training resources to support public health staff who lack data experience.
SHARE-NW was developed with extensive input from rural public health professionals to ensure it meets their needs. Ultimately, it could aid data-driven decision making and bolster requests for funding to improve the health of rural communities.
Pandemic worsens food insecurity for tribal communities

A survey of people from 26 of the 29 federally recognized native tribes in Washington state shows that these communities faced a rise in food insecurity during the COVID-19 pandemic.
Washington’s tribal communities have long faced food insecurity and food access barriers due to the history of colonization and their displacement from native lands. According to the new study, the pandemic exacerbated these challenges through high levels of unemployment and disruptions to traditional food access and gatherings.
The study was part of the ongoing Washington State Tribal Food Project, which is led by researchers at the Northwest Portland Area Indian Health Board, Tacoma Community College and the UW. The research partners worked together again in 2022 to expand the survey to Oregon and Idaho tribes and re-surveyed Washington tribes to learn about changes over time.
“The goal of the project is for trusted tribal leaders, tribal communities, and others with information for advocacy and change to improve food security and well-being in their communities,” said Jennifer Otten, food systems director and associate professor in the UW Department of Environmental & Occupational Health Sciences and the Nutritional Sciences Program. “We’re proud of the work our team did in support of Washington tribal communities.”
