Researchers are using climate data to simulate mosquito populations and their interactions with humans in order to map current and future risk of dengue virus transmission in the United States, according to a new study published this month in Environmental Health Perspectives. The maps suggest that, as climate changes, several areas in the southeastern U.S. may see elevated risk of dengue virus transmission over time.

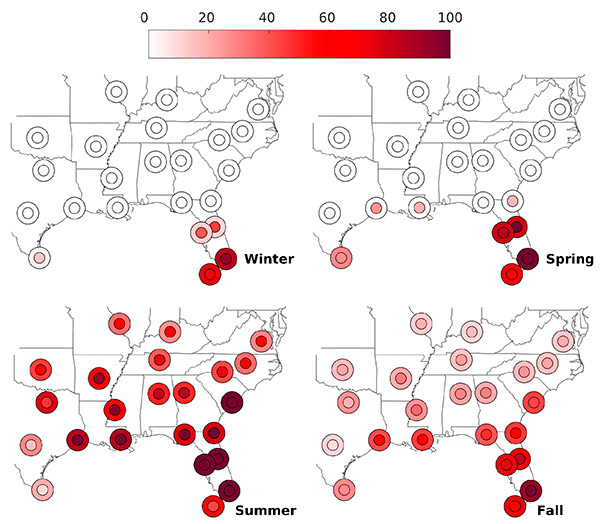
Parts of southern Florida and Texas already have climate suitable for dengue virus transmission and cities such as Atlanta, Birmingham, Charlotte, Dallas, Little Rock, Louisville, Nashville and New Orleans may be at increased risk of transmission in the future. Though risk estimates are highest during the summer, the window during which transmission can occur will extend to the spring and fall for most cities.
“Climate can strongly influence the population dynamics of disease vectors and impact disease ecology,” says Cory Morin, co-author of the study and acting assistant professor of global health at the University of Washington School of Public Health. “It is important to know how transmission risk could change over time, as we will eventually have to shift surveillance and preparation for vector control.”
The study uses daily temperature and precipitation data to simulate Aedes aegypti mosquito populations and virus transmission in 23 cities in the southeastern U.S. The Aedes aegypti mosquito is the main vector that transmits viruses that cause dengue, a viral infection that causes flu-like illness and occasionally develops into a potentially fatal complication called dengue hemorrhagic fever.
The simulation calculates daily development and survival rates as mosquitoes proceed through their life cycles—from egg to larvae, then pupae to adult. It also simulates how the dengue virus is spread to humans via the bite of an infected female mosquito, as well as the incubation period for both the vector and the human. Simulations are based on current weather data and projected climate conditions for the years 2045 to 2065, pulled from a statistical weather generator.
Morin, also a researcher in the School’s Center for Health and the Global Environment, originally developed the mosquito simulation in 2010 to model a species that carries the West Nile virus.
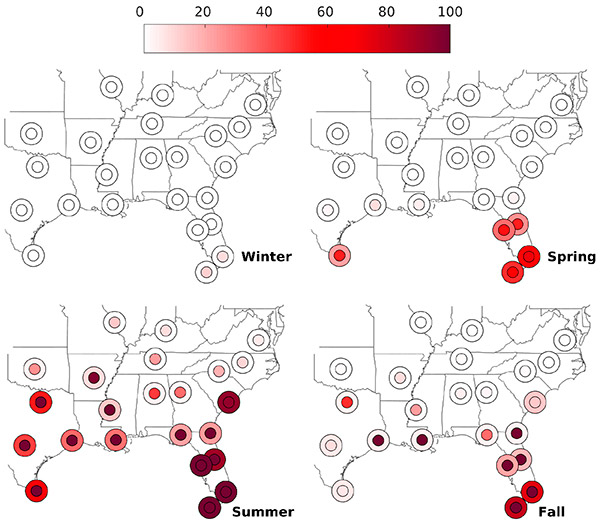
Simulated dengue fever cases in this study are compared to those obtained in a previous study for San Juan, Puerto Rico, where dengue is endemic and the model was evaluated. Simulations that exhibit relatively little or no virus transmission indicate that the U.S. city’s climate is unfavorable for epidemic dengue, while simulations that produce a comparative number of dengue fever cases indicate that climate is conducive for virus transmission. Comparisons were made for both current and projected mosquito populations, and maps were created to show the change of dengue virus transmission risk over time.
Researchers found that the current climate is suitable for virus transmission throughout much of the southeastern U.S. during the summer months (July to September). Parts of southern Florida, including Key West, have the highest likelihood of transmission. Estimates for Brownsville, Texas, indicate a relatively long season where mosquitoes are active and conditions are suitable. These are also the only two locations in the continental U.S. that currently experience locally acquired dengue fever cases.
“Southern Florida already does a lot of vector control, which may need to be extended to earlier in the spring and later in the fall,” Morin says. “Nearby areas in surrounding states, especially in the Gulf, will eventually have to start monitoring for dengue, Chikungunya and Zika.”
Though the current model does not incorporate Chikungunya and Zika specifically, Morin notes, the potential increase in seasonality of Aedes aegypti may impact the transmission of these viruses as well.
Researchers note that U.S. cities will likely not sustain year-round dengue virus transmission due to low winter temperatures that are likely to prevent any permanent establishment. For local transmission to occur, Morin says, the virus would need to be reintroduced each year.
The study’s corresponding author is Melinda Butterworth from the Department of Environmental and Earth Sciences at Willamette University in Oregon. Andrew Comrie from the University of Arizona was also a co-author.
